You’re listening to Burnt Toast!
I’m Virginia Sole-Smith, and today my guest is .
Dr. Gordon is a family physician on the faculty of Cooper Medical School of Rowan University, as well as a writer, journalist, and contributor to NPR. Dr. Gordon also writes
, about her efforts to make medicine more fat friendly, and help her patients and herself explore body liberation and radical bodily autonomy.In our conversation today, Dr. Gordon and I get into why the healthcare system is set up the way it is, and what we can do to advocate for more weight-inclusive care—even when we’re not seeing weight-inclusive doctors.
She also answers your questions about common weight-linked health conditions like acid reflux, sleep apnea, and prediabetes.
PS. If you enjoy today’s conversation, please tap the heart on this post — likes are one of the biggest drivers of traffic from Substack’s Notes, so that’s a super easy, free way to support the show!
Episode 167 Transcript
Mara
I am a family doctor in practice in Camden, New Jersey. That means I take care of both adults and kids and I practice what I like to call size inclusive medicine. I’m also a writer—and I’ve written a fair amount about my interest in making healthcare more fat friendly. And I’m an advocate for making healthcare a more size inclusive space.
Virginia
You are also part of a new organization that was just launched, Association for Weight and Size Inclusive Medicine, which, as soon as you told me about it, I was like, thank God, this finally exists.
Mara
We are so pumped. This organization is called the Association for Weight and Size Inclusive Medicine or AWSIM (pronounced “awesome!”) for short.
Virginia
Oh, just got the acronym!
Mara
You can find us at weightinclusivemedicine.org. Basically we’re a group of physicians, nurse practitioners, and physician assistants who are committed to size inclusive medicine and committed to making healthcare more welcoming place for people who live in bigger bodies.
The need for this is just so obvious. Healthcare spaces are ground zero for fatphobia.
I think they’re often a lot of people’s origin stories for fat phobia, too, which really disturbs me. Like, “my years of body dysmorphia started with an offhand comment from the pediatrician when I was a kid.” Over and over again, I hear these stories, and it is awful. We need to do better.
So AWSIM began as a group of of us who found each other organically online. We’re all over the country, all over the world. Actually, we have some folks in Canada, in South and Central America, but I would say that we’re North America focused for now. We’re trying to build a movement, a professional home for doctors and other healthcare providers who are interested in fighting against fat stigma and making our offices more welcoming spaces.
Virginia
This is so great because one of the questions I’m asked most often is: How do I find a weight inclusive doctor? And there just hasn’t been a place to point people, like an easy answer. And of course, you guys are a new organization. I’m not saying you’re going to solve it for everybody all over the country this minute, but the fact that you are working towards this is really, really thrilling.
Mara
Right now we’re in our really early stages. I’m actually learning so much from our medical student allies. In particular, Medical Students for Size Inclusivity is a grassroots organization that now has chapters all over the country working to start conversations about size inclusivity at the medical school level.
I’m a medical educator. I teach medical students. I love working with them, and MSSI has just done such an amazing job of finding networks, connecting with networks. It’s really community organizing in a digital age, right? They are bringing together a movement of students saying, “Hey professors, you’re doing a terrible job at this. We want better for our education. We want better for our future patients.”
We have a lot of MSSI members in AWSIM, which we hope will be their professional home once they become practicing physicians. I gotta give them credit. They’re just leading the way, and I’m learning so much from them.
Virginia
The reader letters that give me the most hope are the ones from medical students. Because I’m just like, okay, if you get it now you’re going to go into healthcare, and there’s going to be more of you guys doing it that way. That’s so encouraging.
Mara
It’s awesome. And I think eventually, our goal is to one day have a directory of healthcare providers who identify as size inclusive. We’re a long way off from that. That’s a lot of work. But we hope it’ll be a way to organize and build community. It can feel lonely sometimes, advocating for more fat-friendly health care, just because the dogma is so fatphobic.
Virginia
It’s just so stacked against you.
Mara
It is so stacked against us.
I think when I started speaking and writing about some of these issues, my fear was always, somebody’s going to call me stupid, right? Like they’re going to say, oh, haven’t you read all of these studies that show the link between BMI and the risk of all these diseases.
I think we have a culture of fear and shame around asking new questions in medicine.
It’s the fear that you’ll look dumb on rounds, right? Rounds is when all the doctors are standing around, like on House, outside of a patient room, presenting the patient’s case, and everybody chimes in, like, oh, have you heard of this medical study about this? Or, oh, have you thought of this rare disease? In some ways, it’s a great culture, of pushing the team to make sure that we’re doing really, really rigorous science. But there’s also a dark side to it, where we just get really entrenched in dogmatic ways of thinking. There’s always this like, “Oh, you’re dumb. You’re not up to date on the science. You’re not a rigorous scientist,” is always the answer to anything that might question the existing dogma. So it feels great to have a community of support to change that dogma, and trying to question some of the really entrenched ways of thinking in healthcare that are causing a lot of harm to our patients.
Virginia
What helped you connect these dots? Or what was it for you, that moved you? Because I’m assuming your medical school training was this more traditional, dogmatic model.
Mara
Like many philosophical shifts, it wasn’t just one moment, right? I definitely trained in an environment that was very much “lose weight, that will solve all your medical problems.” I wish I could say that I have never practiced that way, but I really have. And I think part of my work in exploring some of these issues is acknowledging that I’ve caused a lot of harm in taking that approach over time.
I was doing what I was taught to do, which is, “Hey, have you thought about hopping on the treadmill more often, that’ll fix your XYZ problem?” And I started to notice over time that it wasn’t working. I noticed that it wasn’t working at the stated goal of weight loss. It wasn’t seeming to prevent complications. It wasn’t preventing disease. And I could see it really doing harm. I could see people’s faces disengage when I brought up topics of body size or weight. They just wouldn’t come back to see me, right?
I could see that I was losing their trust. That was really painful to admit and acknowledge, because that wasn’t why I went to medical school, right? I imagined I’d be a great communicator and my patients would trust me, and we’d have relationships over many years. The fatphobia that I was enacting was not achieving those goals.
Virginia
I love though that you noticed that disengagement and thought, Wait, what am I doing that’s contributing to that?” So often what fat folks experience is that if we disengage, the doctor then labels us as noncompliant or hostile. We’re just not trying, we’re not taking it seriously. The fact that you were like, “Oh, wait a second, if the patient is disengaging, how am I losing them?” That’s a really different shift.
Mara
I didn’t do it alone. I think reading works by fat authors really helped me start to think of these questions in broader ways. Reading the work of
, and Kiese Laymon, —all those books which I read maybe like five, seven years ago started getting me thinking about some of these issues.And I mean, honestly, my own body changing, right? Around pregnancy and childbirth—I have a three year old son—I got fatter. And realizing that the advice I was doling out, I couldn’t take myself. I started to realize maybe the advice is bad. Maybe it’s not me, right? Which is a really profound shift in in thinking that takes time. And it takes thinking about these questions and talking about these questions over and over again.
So it’s been a slow, slow process, but it feels really exciting to be part of a community that I hope is really changing things for the better and trying to do good in pretty disastrous healthcare system, in a healthcare system that perpetuates a lot of harm.
Virginia
We can only go up at this point, right?
Mara
I know.
Virginia
So that’s what you’re not doing anymore in terms of pushing weight loss as a blanket prescription when you’re seeing a patient. What are some other things you do differently now? What does practicing size-inclusive medicine look like?
Mara
I joke that size-inclusive medicine is basically not yelling at my patients to lose weight.
Virginia
I love that.
Mara
It’s so basic, and yet, everyone has had an experience with this, right? I always come back to this, too. I have thin friends who tell me, “Oh my gosh, I won’t wear a sweater or boots when I go to the doctor because I don’t want to get weighed and tip over into that 26 BMI and all of a sudden feel that wrath.” Like the reams of paperwork you get that are like, here’s how to lose weight, and your BMI is flashing red in the computer.
So at the core, I don’t yell at my patients to lose weight. Reading some of the scientific literature about the inefficacy of diet and exercise for weight loss is what got me interested in this more size inclusive approach. I was like, wow. This thing that I’m doing—counseling my patients to lose weight—isn’t working. That’s really borne out in the literature.
Weight counseling intervention in primary care medicine has pretty much zero data to support it.
So I was doing this thing that had no evidence base. I would never prescribe a medicine that didn’t work, right? So that’s what got me interested, and I started learning about it. I am a huge fan of exercise. I know that many folks listening to the podcast may find exercise triggering or harmful for whatever reasons, and that’s totally fine. You have no moral obligation to exercise. But I find it really helpful in my own life, and many of my patients find it really helpful in their lives.
So what I say now is, “Actually, I don’t care if you lose weight, but I do care that you exercise.” It’s it’s really shifted my focus from a weight goal or a BMI goal, for my patients and for myself, frankly, to what are these healthy behaviors that we can engage in on a regular basis?
For most people, that’s regular exercise, sleep, stress reduction. You know, all these things that we think of as really helpful for wellbeing. And now I just don’t care if they make you lose weight, I care that you’re doing them.
I think that’s also borne out in the literature. I mean, we really see there is research on this that’s really interesting, which shows that people get cardiovascular benefits and metabolic benefits from regular exercise, even if they don’t lose weight. So I don’t care what the number on the scale is. But let’s talk about these routines you can have in your life, or these medications you can take, frankly, because I do think that access to healthcare. Access to medications is a big part of it for some people.
There are these things that you can do on a regular basis to try to achieve whatever feels healthy to you, right? What your definition of of healthy is.
Virginia
I would imagine, too, that decoupling exercise from weight loss allows you to talk about exercise in a more nuanced way. Because if we’re assuming the goal of exercise is weight loss, then there’s only one way to exercise, or like a fairly narrow definition. It’s as much cardio as possible, as hard as possible, and always more and more or whatever. This approach would allow you to then talk to people about, what’s doable in your life, and what do you enjoy? If it doesn’t matter whether it makes you lose weight, there are more options on the table, and then there are more ways people move their bodies.
Mara
I will say, this is something I really struggle with clinically. We have these 20 minute visits. And a lot of my patients are not radicalized towards body acceptance. They are just every day people showing up, making comments on their weight, making comments like, “Oh am I a healthy weight doc? Oh, I gained five pounds, doc.” So it is really challenging. When I say the word exercise, I think a lot of my patients hear weight loss. So part of the work that I’m trying to do is to undo that.
Virginia
Yeah, that’s tricky.
Mara
It’s hard in our tiny little 20 minute visits. But I’m curious to hear from you, though, Virginia. What has helped you start to detangle exercise from weight loss as a goal?
Virginia
That’s a great question. I did have to put exercise down for a few years in order to not do it compulsively. That is part of my history. And running would probably not be prescribed to me, or should not be, given the way I ran in my 20s.
Mara
Running is a lot.
Virginia
Love it for other people, really not my jam. But anyway, after having kids I developed a lot of back pain. And I realized that strength training is the one thing that really keeps my back on track. I mean, I realized this, to be honest, after quite a few experiences of falling off the strength training wagon, throwing my back out, ending up in physical therapy again. I had to learn that lesson a few times.
Mara
Yeah, totally.
Virginia
But now, it’s oh, if I do this, I can prevent this immediately life-derailing pain problem that I have. It is not fun to throw your back out.
Mara
Yeah, it is not. It is not.
Virginia
And it has nothing to do with weight. It’s just like, if I don’t do this regularly, I will throw my back out every six months, and I don’t need that in my life. So for me, it was replacing weight with another tangible benefit. I can see that a equals b here. And obviously I hope most people don’t have back problems. But I do think finding some immediate benefit from exercise that you can hold onto really helps. Because a lot of us are just like, “I’m not someone who loves exercise. I don’t get an immediate endorphin high off it.” It doesn’t do for me what it does for some people. I get an endorphin high from, like, reading a book on the couch for four hours, not going for a hike.
Mara
Yeah, totally. And that’s okay!
Virginia
I don’t have that internal motivation. So I did need an external motivator, but it needed to be an achievable external motivator, which weight loss never was.
Mara
Yeah, that’s so well said. I think that is what I’m hoping for for my patients. And honestly, I’ve experienced it, too. When I was pregnant, I had terrible insomnia, which, thank God, is something that I don’t experience while not pregnant. And I was really struggling to exercise while I was pregnant, and that was what motivated me. It’s like, oh my gosh, this is going to help me sleep, right? And that was the main thing that got me going again.
There are these ways that movement can make you feel healthy that just completely take weight out of the equation. And that’s my goal as a doctor, which is tough, because I think we have such entrenched ideas about exercise and weight loss. And frankly, even when I start to say, like, “exercise can help with diabetes prevention,” you know, the word diabetes is very much associated with being fat. And it’s not entirely! I have a lot of thin patients with very advanced diabetes. It’s really humbling how hard it is to predict who’s going to have severe disease and who doesn’t.
But anyway, I think my goal is to disentangle the the practice that can have very real health benefits from some of this stuff we’ve gotten mixed up with weight loss.
Ask Dr. Mara!
Virginia
Well, since you brought up diabetes, that’s a perfect segue, because we’ve been gathering some “Ask Dr Mara” questions from the community.
Mara
I can do my best!
Virginia
Now to be clear, Mara Gordon is not your doctor. She is not giving you individual medical advice. All the disclaimers. She’s going to talk generally about weight and health that will be useful to a lot of us. But here’s the first question:
What’s the deal with prediabetes? Is this a real condition or just a stick to beat fat people with?
Which I was like, well said.
Mara
So I think my answer to all of these is going to be, we don’t know, right? I did a little bit of homework in preparation to answer this question. Thank you to the listener who asked it! But I’m a little disappointed with the results, because we just don’t know the answer.
I looked up prediabetes in Cochrane Review, which is published by Cochrane Database, a nonprofit research organization that summarizes medical evidence. It’s where I turn to when I have a big philosophical clinical question.. And I found what’s called a systematic review about your risk of developing diabetes if you’re diagnosed with “prediabetes.” They found over 100 studies, and they summarized them, and analyzed them together, and the short answer is: We have no clue.
Virginia
A hundred studies and we know nothing.
Mara
Part of what makes it so hard to study is that we don’t have consistent definitions of what it means to have prediabetes, right?
Virginia
Oh cool. That wouldn’t be useful at all.
Mara
The lab I use in my clinic will tell people they have prediabetes constantly. I mean, this happens on a daily basis for me. Our lab uses a cutoff that’s defined by the American Diabetes Association, which is a great organization. They do a lot of amazing research. They also take a lot of money from pharmaceutical companies, and often are criticized for trying to get more people on more medications. But they also do great work. I mean, again, it’s complicated, right?
So my lab uses the ADA definition of prediabetes so my patients, when they get a diabetes test done, the lab will tell them, on the patient portal, the app you have from your doctor, it will automatically get sent to them before I’ve even looked at the results. And have a moment to be like, wait, wait, wait, let me explain. And it will just pop up red saying “you have prediabetes.”
Virginia
Oh God. And everyone panics.
Mara
Totally, but that definition is from 2001, from the American Diabetes Association. And it’s a hemoglobin A1C level in a certain range. We won’t get too much into the weeds, but basically that’s a measure of your blood sugar over the last three to four months. And it’s a really useful test. I use it daily in my clinical practice.
But the ADA, in 2001, was like, okay, we think we’ve agreed the definition of diabetes is this number, a hemoglobin, A1C over this. And we’re going to say that prediabetes is between a different range, right? But the World Health Organization disagrees, and says, hey, actually, the ADA definition is not appropriate.
And there are also all these different European and international diabetes organizations, and we can really get into the weeds, and they all debate what prediabetes is, right? It’s crazy.
So long story short, going back to the review that I looked at: Even trying to have some cohesion about these different definitions of what it means to have prediabetes is difficult. We don’t have a great sense of who goes on to progress to true diabetes, and who regresses to what we call normal glycemia, like their blood sugar normalizes.
It seems like people who use a higher cutoff for prediabetes tend to have a higher risk of developing prediabetes than a lower cutoff. More of those people go back to normal glucose levels. But it’s all a mess. It’s wild.
Virginia
Right, because they might have gone back to lower normal glucose levels because they were never really at risk.
Mara
Totally. There is harm in making the cutoff too low. And this is a really interesting question in medicine in general, which is you know, if you make a threshold for positive tests lower, you catch more people, right? But you also have more false positives.
This is something we teach our medical students in first year of medical school, like, thinking about appropriate thresholds for positive versus negative tests. And I don’t know what to make of it.
I mean, what I tell my patients, because they come in like, “Oh my God, Dr. Gordon, now I have prediabetes. Like, what does this mean? Am I dying?” And I’m like, “I don’t know.” We don’t know really what it means. I usually don’t recommend that we start a medication. Although I have patients who want to, which is maybe a separate issue. I’m like, you know what? Let’s focus on regular exercise. So it’s what I’ve been saying all along. A prediabetes diagnosis doesn’t really change my recommendation in the end. That was a long-winded answer, but it’s a really complicated question it turns out.
Virginia
It’s so complicated! But you know, to distill it down a little bit, I think this listener is right. This label can be weaponized against fat folks. Because they’ll put the prediabetes label on your chart, and then a doctor will use that to be like, “Okay, we need to lose weight.” We need to push this agenda.
And a different way of thinking about it is: Here is a data point that we don’t really know what to do with. But let’s go back to talking about healthy lifestyle, and how that will benefit you regardless of whether your weight changes. To reframe the power of that label, I think is really important.
Mara
Yeah, and diabetes is a disease that’s just so highly stigmatized, and it is really common, and yet this shame around body size and diabetes just really, really persists.
I mean, I’m just humbled—the further I get in clinical practice, I cannot predict who’s going to have diabetes and who isn’t. I think the most predictive thing is family history. There’s just something genetic going on that’s putting people at risk. And, I mean, the stigma does so much harm, right? People are afraid to seek care. They’re embarrassed to seek care.
We know from so much research that the more stigmatized a condition is, the worse people do with it.
So prediabetes—I wish it didn’t exist, long story short. It’s not totally clear if it is useful in predicting your risk of future diabetes. A lot of people revert back to so called normal glucose levels, and I don’t really know what to do with it.
Virginia
I think that’s an honest and actually really useful answer, just because it takes the fear down a little bit for anyone who gets that diagnosis, having this larger context is is useful. It’s not as black and white as they think.
Mara
It is not. Few things are, so few things are in healthcare.
Virginia
Two other conditions that we got questions about are acid reflux and sleep apnea. So I thought we could talk a little bit about each of those.
On the acid reflux front, this person wrote, “I was recently told that if I even lost five pounds, my acid reflux would be cured. Is acid reflux actually caused by my excess weight pressing on my esophagus?”
Mara
I’m so sorry you have acid reflux. It can really suck.
Virginia
It really does. Solidarity. I also have it.
Mara
I mean, the short answer is, again, it’s complicated.
But the longer answer is a good doctor is going to find ways to help treat your conditions that feel concordant with your health goals. So if thinking about weight is an unhealthy practice for you, a good doctor is going to avoid it, right? There are great treatments for heartburn, for acid reflux, that do not involve weight loss. Really handy medications you can buy at WalMart or Costco that really, really help. They’re great. Modern medicine can help get rid of your heartburn.
I have some patients who do really want to lose weight, and that is concordant with their health goals. And, of course, it’s informed by culture, right? It’s informed by our fatphobic society. It’s informed by our fatphobic medical culture. But you know, I have patients who say, “Oh, I lost weight and my heartburn got a lot better.” And I have patients who are really, really thin, who have terrible heartburn.
So I think the answer is, there’s no one size fits all approach. It’s really about the patient who’s in front of me. It’s hard to answer that question in a blanket statement, but I think it’s really about defining what your health goals are. And if it feels unhealthy to think about weight like it does for many of us—it feels that way for me, then let’s find a different treatment plan. There’s plenty of them, right?
Virginia
Yes. And this doctor who said, if you even lose five pounds, it will be cured—Like, that’s clearly an overpromise. Like, how could that person be so certain?
Mara
I mean, there are just so many horrific offhand fatphobic statements that I hear secondhand all the time. I mean, that’s just ridiculous, that’s just wrong.
Virginia
I’m assuming it’s a similar conversation with sleep apnea. You have some folks who find a little bit of weight loss benefits. You have other folks who are thin are struggling with it. That seems to be a recurring theme here, right?
Mara
Totally, right. There are absolutely thin people who get sleep apnea. Kids get sleep apnea! Children should be gaining weight. Their bodies are growing. And we see all the time we have kids who have severe sleep apnea, and the treatment for that is actually getting their tonsils out, right?
For adults, again, it really varies. I have patients of all body sizes who have sleep apnea. I think sometimes people tell me, like, “Hey, losing losing some weight has helped my sleep apnea.” And, I have people who can’t lose weight or don’t want to lose weight, and we find other treatments for them. Again, it’s really about defining the patient’s goals and trying to treat each condition objectively, without a focus on weight as my goal, as a size inclusive doctor.
Virginia
That’s a super helpful reframing.
Is there literally any health issue for which weight loss is indicated as a necessary treatment?
Mara
Is there ever a time where I tell a patient that the only thing we can do is weight loss? The answer is no. I mean, that’s just not patient centered care.
Unfortunately, a lot of doctors disagree. I hear stories all the time of people who say, “the doctor told me the only treatment for my knee pain was to lose weight, or the only treatment for my heartburn was to lose weight.” Like, you can go buy some Nexium at Costco, right? I do think it gets framed in these sort of hyperbolic terms.
So, yeah, I will put my stake down and say, no. There is no condition where the only thing you can do is lose weight.
But I do think that there are circumstances where people derive benefit from weight loss. And I think that’s a really subtle point that I sometimes struggle to get across as a size inclusive doctor. It’s not a moral obligation. It’s not a medical necessity, but a lot of my patients want to lose weight, and often people feel like their conditions have improved when they lose weight. But, a lot of people don’t want to lose weight, and we find other ways to treat their conditions.
And remember, a lot of people are pretty thin to begin with, and they still have medical problems. So I try to use that thought exercise of, what would I recommend to somebody who had a BMI of 24? That’s a helpful approach for me as a doctor to think, I wouldn’t be recommending weight loss to somebody who had a really low BMI. So how can we think more expansively about other treatments for all patients?
But you know, when I first started talking publicly about size inclusive medicine, it was in the context of Ozempic coming on the scene. And I just had patients in droves coming to see me saying, “Hey, you’re a size inclusive doctor. Like, can you give me Ozempic, right?” And I was like, wait, were you listening to what I was saying?
Virginia
I don’t think you understood the definition?
Mara
Totally. And at first, I mean, I sort of experimented with, I don’t know exactly, not quite withholding the medication, but… I quickly found that it was not therapeutic to act as a gatekeeper. I wouldn’t do that for other types of medications. Like, oh, I know better than you what your body needs. I mean, I do in some ways, because I went to school for a long time. But, I don’t, in the sense that you know your body much better than I do. I found that having a really dogmatic “I won’t even engage conversations about weight” approach with my patients, is not therapeutic, in the same way that yelling at them to lose weight is also not therapeutic.
Virginia
Well, and it’s not supporting their body autonomy.
Mara
Exactly, right? And that’s the core of everything is bodily autonomy.
Virginia
When you do have a diagnosis that is associated with being at a higher weight, whether it’s one of the ones we’ve already talked about, or cholesterol, blood pressure, etc, what is the best way to discuss those conditions without a focus on weight loss as a first step?
Mara
I actually had a patient who came to see me specifically because she had a history of pretty severe eating disorder and she didn’t want to get weighed. We didn’t weigh her, but she wanted to get blood work. And she came back with her cholesterol mildly elevated. And she was really upset when she got those test results, and was like, “Oh my gosh. I’m working so hard to heal from my eating disorder. What does this mean? Does this mean I have to go on a diet?” And it really challenged me to think, like, okay, how can we be holistic about trying to help patients understand what their test results mean, or preventing disease or treating a disease that they’ve already been diagnosed with.
And the answer is that there are a lot of treatments other than weight loss, basically. So, there are medications. There is regular movement. You know, diet is complicated, and maybe we can set that aside for a bit, because that’s that’s a really complicated can of worms. But there are ways to minimize your risk of developing disease or treating disease that don’t focus on weight loss.
I think if you’re seeing a doctor who isn’t used to thinking about it in a more size, inclusive way, I think just starting with feeling comfortable advocating for yourself and your health goals is always the first advice that I give people. I think most doctors really want to do the right thing. We haven’t always been trained to do it in a way that is concordant with bodily autonomy and size neutral approach. But I think they want to do right by their patients.
So I think really clear, direct communication about, “I don’t want to talk about my BMI.” Like, that’s not something that’s on the table for discussion. I think most doctors will greet it, maybe not enthusiastically, but at least will be respectful of a patient’s desire.
Clear communication is the first step if it’s important for you to talk about a diagnosis that’s traditionally been associated with a higher weight with your doctor, and the doctor isn’t quite yet on board.
Virginia
That’s really helpful and I think empowering for people to know that, if a doctor has your best interests at heart, they should be open to taking the conversation in that direction. Unfortunately, depending where you live, you can’t just fire a doctor and find a new one the next day. But it’s so easy, as the patient, to feel vulnerable and feel like I have to listen to whatever this person is telling me. So just underscoring for folks that you have the right to say, no, I want to handle this differently, I think is really, really useful.
Mara
Yeah, totally. I guess I’m curious to hear from you, from your readers, Virginia. I’m sure people contact you about this all the time, and what, what do they say? I give this advice, like, you know, speak up for yourself. But I think the power dynamic—I do underestimate it sometimes because it’s my day to day.
Virginia
It’s a real range. I definitely hear from folks, and I have found myself, that when you do advocate for yourself, you can often be pleasantly surprised by the results of a doctor being willing to move the needle, and reframe and meet you where you are. And that’s great. And it’s worth trying.
And I think there’s also the reality that it’s easier for me as a well-off white lady with a lot of education to go into a room and say, I want to handle it like this than it is for a person of color. The more barriers that you’re encountering, the more barriers you’re encountering. And so that’s just the tough thing about it.
I think for a lot of folks the reality is that they have to play the weight game with the doctor because that’s how they access the care they need for other things. You’re not going to put up a big fight about not getting on the scale because you need to be perceived as compliant during the appointment. There’s just a lot of nuance to this. But I do think that core of like reminding people that they should have this power, even if it’s not always readily available, is still valuable.
Mara
I mean, the onus is on us, right? Meaning me and my doctor friends. I don’t mean to shift the blame to patients, like, “If you just speak up more, it’ll all be fixed.” Because it’s really, really complicated. I mean, that’s part of the advocacy work that I’m doing is trying to change these conversations within healthcare.
Virginia
Okay, one last listener question.
What is the best resource to point different health professionals to to explain why they shouldn’t need to take my weight. I feel comfortable in explaining why I don’t want to step on the scale, but I’d love to use those few seconds to broaden my potential impact on them.
I do want to underscore again that for more marginalized folks, refusing to be weighed often isn’t the mountain to die on. Like you get on the scale, because you don’t want to pick this battle.
However, I personally don’t get on scales anymore. If you’re in eating disorder recovery, it’s not necessarily safe for you to be on a scale. And I also think for thin folks going to doctors, this can be a great advocacy opportunity. Use your thin privilege. Don’t get on the scale and tell them why.
So I’d love your thoughts on what should this person say? Or what can they point their providers to.
Mara
I’ll say, like, hard yes to all of this. I don’t require my patients to get weighed. I don’t know if I ever really thought about requiring it. It’s just such a part of the intake process, right? I mean, it’s just this ritualized gauntlet, right? I mean, nobody likes it. It’s awful. And it harms thin people, too. I just think about my friend talking about not wearing boots to the doctor. I mean, how silly. And just the mental space wasted on that.
Working in a big hospital system, it’s hard to change a workflow that’s really, really ingrained. And I actually have done a little bit of reading, I was sort of curious, do we have data to show that it’s actually safe to completely forgo weighing all of our patients? And I don’t think we know the answer. It just it hasn’t really been studied.
I think particularly in children, it worries me a little bit, because kids really should be growing. And I think there are some circumstances in adults where it makes me a little nervous, too. Particularly around rapid weight loss. I practice in a low income, in a community of color, most of my patients are publicly insured, and my patients have a lot of stress in their lives, and they’re not like lining up to get their mammograms and their colonoscopies, right?
All this is to say that rapid weight loss can be—I don’t want to use the term cancer screening. I mean, that’s not the right way of thinking about it. But my patients aren’t getting all the preventative care they should be getting, so that’s one additional clue if they’re losing weight rapidly that I should be digging into what’s going on with them.
So I have mixed feelings about it. I have some patients who don’t want to be weighed because of a history of disordered eating, and I’ve never weighed, and I’m fine with that. But it’s not my practice to just completely forgo weights completely for everybody. I just don’t know if there’s data on whether or not this should be a universal practice where we just give up weighing all adults or not.
To the listener, I wonder if some of the eating disorder literature on harms of a public weighing process around people who are in recovery from eating disorders might be compelling or interesting to their doctor. That was sort of my first thought. There are known mental health harms to being weighed, often in public. I mean, just in the middle of the dang office, it’s so ridiculous, and in front of your family members. I mean, it’s just so bad.
But my second thought is, I love it when my patients bring me stuff, whether it’s like scientific papers or stuff they’ve read in the news. But I felt like the subtext of that reader’s question was also like, “oh, I think that this is going to, like, convince my doctor to change.”
Our visits are just so short. But what’s coming to mind is some of the literature about, like, decision making around vaccines, right? When my patients don’t want to get a vaccine, I used to be like, oh, look at all this data about why you should vaccinate and get the COVID shot and whatever. And I just don’t think people in these tense emotional moments—they don’t respond to data like that. I would hope a doctor has enough training to rise above it, but I think we’re humans too. Doctors are people. And I worry that sort of, oh, look at this thing that you’re doing. Here’s all the data why it’s wrong is not the way that people change their mind about behavior.
Virginia
I agree.
Mara
And I think doctors should hold ourselves to a higher standard because of our position of power in in that decision making process in the exam room.
But I wonder if maybe a more emotional approach actually is the way to affect change in the same way that when I talk to families about the COVID shot, or their flu shot, I say, “I just took my three year old to get his flu shot last week. I don’t say like, oh well, there’s a 57% blah blah rate.”
So anyway, again, not that it’s the listeners responsibility to fix health care, but I’m sort of curious about whether a personal story or a more emotional approach about why they experience harm from being weighed might be an interesting way to explore it.
Virginia
As a journalist, I obviously believe in the power of personal stories to affect change. It’s my whole raison d’etre, so I’m a fan. I do think there is a risk that we often go into healthcare settings already defensive and combative, and that does not serve the goal of affecting change in healthcare. Nor does it generally serve our own health.
And again, as you keep saying, it’s not the responsibility of patients to make this change happen. But if you are someone with privilege who feels like, oh, I could work towards getting this healthcare provider to think more expansively about these topics, then probably building a rapport with that person will get you further. It may not happen quickly, but building that rapport will help you over time open up the discussion a little more.
Mara
Totally, it’s about relationship building and and I mean, doctors are humans. And I get this question a lot, like, why are doctors just so bad at this? I mean, the answer is super complicated. But, I think the answer is that we’re humans and we’re products of a fatphobic culture, right? And as much as we like to think that medicine is objective, it’s obviously not. The questions we ask in medicine, the research we do in medicine, is defined and influenced by culture, and our culture has a lot of work to do.
Butter
Mara
Oh my gosh. Virginia, I have been thinking about this all weekend! I am an avid fan of your podcast. I’ve gotten so many good recs from the Butter. And I was like, I need a good Butter. No pressure.
Virginia
I know, people come in very stressed out about it, if they listen to the show. But we love a random butter. It doesn’t need to be anything mind blowing.
Mara
Totally. I guess mine is a little mind blowing. I would like to recommend the book of poetry called What Kind of Woman by Kate Baer.
Virginia
So good.
Mara
So I bought this book, I bought the audiobook in 2020 and when it first came out, and it was pandemic times. I would listen to the audiobook while I would go on these long walks with my dog, because there’s nothing else to do. I would just weep in the streets. Like, it’s just so good, and it has resurfaced in my life, because my book club—shout out to the Badass Women Book Club of the Greater Philadelphia Area.
Virginia
Great book club name.
Mara
Thank you. We chose that book and we just met over the weekend to discuss it, and revisiting it was really wonderful. A couple thoughts, just super briefly. Audiobook form for poetry is the best, because I have a lot of baggage about being smart enough to properly read poetry. When you listen to it, you get the emotional valence of it, you know? And right now we’re recording two weeks before the election.
Virginia
It is now, listeners, two days after the election. I hope we are in a better world.
Mara
I know. Please, Americans of the future, make the right decision. You can do it, guys. I trust you.
Virginia
I hope this episode is reaching everyone in a in a happier place.
[Post-recording note: Obviously fucking not!!!!!]
Mara
Oh, my God, I know. I feel my heart racing. But anyway, Kate Baer’s poetry is about so much about bodies, and feminism and bodily autonomy, and it just feels very prescient. So, yeah, yes, that’s my Butter. Thank you. What’s yours?
Virginia
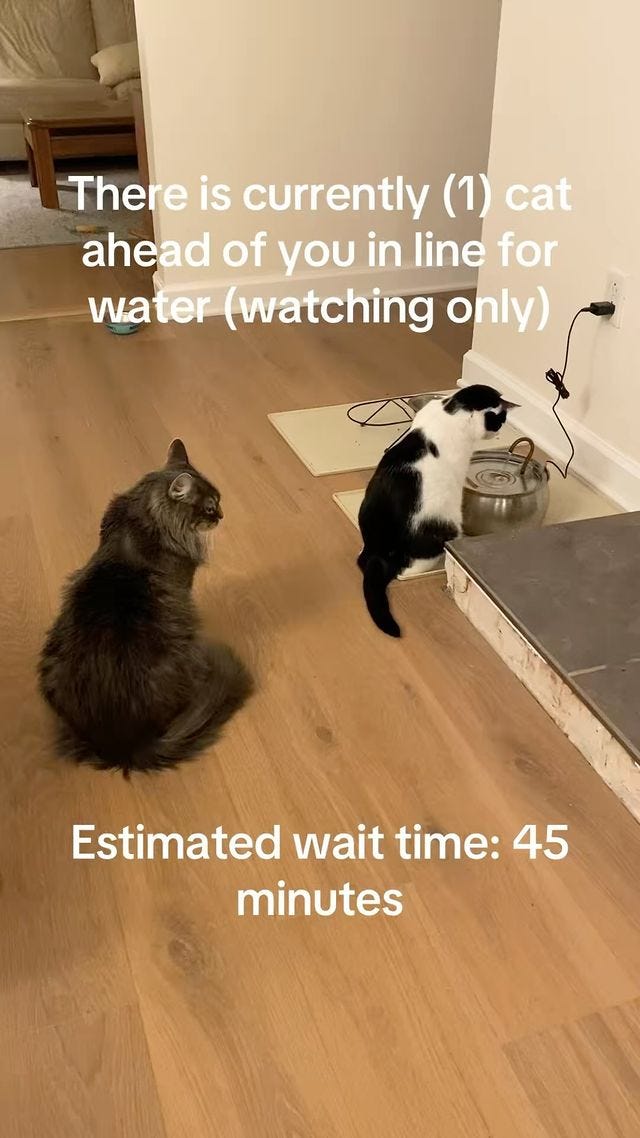
Mine is not as powerful, but still very fun, which is, I am going to recommend watching cat videos with your kids, especially if you have a tween who is hard to communicate with in other ways. The love language of my 11 year old and I right now is dumb Instagram reel is about cats. It is such a mood reset. If things are a little bit stressful, I’ll be like, do you want to see a funny cat? And she’s like, yes. And then we watch a funny cat video, and I will put in the transcript some of our favorites.
My algorithm is now almost exclusively serving me cat videos, which is a great hack for Instagram, let me tell you.
Mara
Thats one way to avoid all horrible content is just click on the cats.
Virginia
Now getting the guy who wears his cat in a Baby Bjorn and the cat’s wearing a funny hat, that’s all I want. That’s all I need to get through—again, listeners of the future, you know what’s happened, but it is a high stress time. I need a steady stream of cat videos.
Mara
I love it. I love it.
Virginia
And it just, it makes me reflect a little bit on how sometimes these gold standard health messages about screen time or phones, all these things. It’s often worth thinking like, but how does it serve me? Being able to use technology to create this bond with my kid, to destress a little bit, it’s just great. It’s great.
Mara
I love that framing, right? You found it to be really positive in your life right now. And that’s fab.
Virginia
And you know, you don’t have to do cats. I’ve also gotten into funny cow videos, is another genre I’m exploring. Like, a video of a woman giving a cow a shower in her bathroom. I don’t know, it’s delightful.
Mara
How’d she get it in there?
Virginia
It’s a small cow, big shower. I don’t know, it brings us a lot of joy. If you’re having a hard week, you probably need to watch a cow take a shower is what I’m telling you.
Mara
Amazing. I can’t wait. I’m going to go look it up right now.
Virginia
Well, Mara, this was fantastic. Thank you again. Tell folks where they can find you and how we can support your work.
Mara
Thank you so much, Virginia. Such a pleasure and I’m such a fan. You can find me on the internet, at MaraGordonMD.com. I’ve pretty recently joined Instagram. It is a kind of cool place. I was resistant for years, but I’m at Mara Gordon MD, and I write a Substack that’s called
. Thank you.Virginia
Fantastic. Thanks again for doing this.
Mara
Thanks for everything, Virginia.
The Burnt Toast Podcast is produced and hosted by Virginia Sole-Smith (follow me on Instagram) and Corinne Fay, who runs @SellTradePlus, and Big Undies—subscribe for 20% off!
The Burnt Toast logo is by Deanna Lowe.
Our theme music is by Farideh.
Tommy Harron is our audio engineer.
Thanks for listening and for supporting anti-diet, body liberation journalism!


















Share this post