Hello and welcome to another audio version of Burnt Toast!
This is a newsletter where we explore questions (and some answers) around fatphobia, diet culture, parenting, and health. I am Virginia Sole-Smith. I’m a journalist who covers weight stigma and diet culture, and I’m the author of The Eating Instinct and the forthcoming Fat Kid Phobia.
Today, I’m pleased to be chatting with Dr. Rachel Millner, a psychologist based in Newtown, Pennsylvania who specializes in eating disorders. Welcome, Rachel! I’m so excited to talk to you. Before we dive into our big topic, why don’t you tell our listeners a little more about yourself and your work?
Rachel
As you already said, I’m a psychologist, outside of Philadelphia, I’m in private practice here. I work primarily with folks who are dealing with eating disorders, disordered eating, those wanting to heal their relationship with food and body. I do a lot of work around anti fat bias and weight stigma. And I frequently talk about “atypical anorexia” and weight stigma and how those issues play out within the eating disorder field.
Virginia
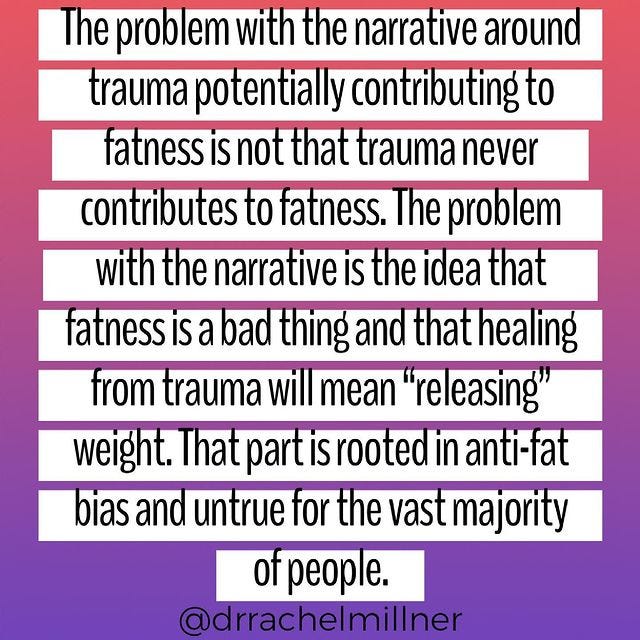
And you have an awesome Instagram that I will link to in the transcript. I also interviewed you for a New York Times piece last year. (And this Good Housekeeping story!) What I wanted to chat with you about today, what kind of inspired this conversation, is an Instagram post you did back in June, and I’ll just read the text here. You wrote:
And I sort of had a real like, yes moment reading this. I think this probably resonated with a lot of folks, and for other folks, this might be sort of confusing. There are a lot of misconceptions about the relationship between trauma and weight. There’s just a lot we can unpack here.
So first, I would love to hear a little bit of the background of what inspired this post for you.
Rachel
I think, you know, there is so much nuance here. And it’s one of those topics that I think does bring up a lot for people, because of all the weight stigma. You know that when we start a conversation around trauma and fatness, given the weight stigma in the culture, of course, we all kind of go into high alert and brace ourselves for like, okay, what’s coming next? What prompted this Instagram post was just sitting with clients and hearing their stories and feeling like their stories aren’t being told. And wanting to name that for some people, there might be a connection between fatness and trauma.
The other side of that narrative that’s so harmful, is this idea that if we heal trauma, then somehow we’re magically not going to be fat anymore. This is something that’s projected onto my clients all the time. So I was just thinking about these conversations that I have in my office all the time, that are never told.
Virginia
I’ve heard this from readers before, where they almost feel like they’re being a “bad fatty” if they say, “I think my body size is related to this experience I had.” That really denies their truth. And it makes it difficult for them to tell their story.
I mean, it gets really messy, it gets really messy. So, I guess, you know, for folks who are newer to this conversation, it might be useful to start by talking about some of those relationships you’re seeing among your clients? How does trauma sometimes relate to body size? What scenarios are you kind of referencing here?
Rachel
The story that I hear from my clients is that when they were going through trauma, particularly childhood trauma, although I think it’s also true for people who have experienced trauma as an adult, that oftentimes food is what’s available to cope. If somebody is in a home where they’re being traumatized, or a child who doesn’t have access to therapy or other ways of getting support, food is often available. And it’s a really effective coping mechanism. It can be really helpful to eat in response to sadness or pain or suffering. And for some people, that eating may lead to weight gain, not for everybody, but there’s, you know, people who, that eating in response to emotions over time might lead to them gaining weight.
Then too, I think for a lot of people who have trauma around weight stigma, and are put on diets at a very young age, we know that dieting often leads to weight gain. A lot of my clients talk about what it was like to have trauma around weight stigma, being told that their body was wrong at a young age, and being forced to restrict their food intake, which then, of course, leads to bingeing and leads to weight gain.
Virginia
Another narrative I often hear about is what Roxane Gay wrote about in Hunger. She framed it as almost more of a deliberate decision to eat as a form of protection. What are your thoughts are on that, if that’s something you also see coming up for folks?
Rachel
I appreciated Roxane Gay’s book so much, because I think this is a narrative that doesn’t get told. And I’m really of the belief that we need to believe people. And you know, when people share their story, we can trust that what they’re saying is true and real. When I have clients who talk about intentionally gaining weight, or thinking about fatness as a way to be protected from the male gaze, that makes a lot of sense. And we still know that that’s rooted in weight stigma. Because this idea that if we’re in bigger bodies, then men are not going to be attracted to us is rooted in weight stigma. And it’s real, right? This is the water that we swim in. It doesn’t mean, you know—there are many people in fat bodies who are in wonderful relationships and have lots of people that are attracted to them. But I think this idea, especially, I hear a lot with my clients who have had sexual trauma, is that there’s a feeling of protection when their body is bigger.
Virginia
Right, that somehow they can hide more that way. Which, yes, again, there’s the layers of fatphobia built right into that, but it’s also an understandable path to seek when you’re struggling in that way.
Rachel
And we know that when people either lose weight, or their body is smaller that, especially for those socialized female, oftentimes their body is sexualized, is put on display, people feel free to comment and you know, “compliment.” And that can be really vulnerable for people, for anybody, but especially people who have trauma history, especially around sexual trauma.
Virginia
I think that’s really important to articulate. The more you’re talking about this, the more I’m realizing how weight stigma plays into it right from the beginning, for so many folks navigating trauma and weight. Even, as you were saying earlier, that the sort of idea of emotional eating, getting demonized, that’s something we talk about a lot here—I’ve certainly experienced it myself. We tend to praise the idea of people losing their appetites while undergoing trauma, like that gets celebrated as if that was a good coping strategy, when actually, that’s quite alarming. That weight loss that can result, again, doesn’t always result but sometimes results, isn’t a good thing.
I remember when my daughter went through a lot of intensive medical experiences, and we lived in a hospital for weeks and months at a time at various points. And people would always sort of encourage me to get out and go for a walk, like that’s what you should do as a “healthy coping strategy.” And I was like, hey, I can’t leave her hospital room. We live here. And I’m terrified if I leave, she’ll stop breathing. So no, I’m not going for a walk. And actually, eating Au Bon Pain chocolate croissants while I sat in this hospital room for hours a day like felt good, and was comforting and it alleviated boredom and stress. I just remember wondering, through that trauma, why is my chosen coping method feeling wrong to everybody around me? And that’s weight stigma. It’s because they didn’t see it as “healthy” because it might result in weight gain, or did result in weight gain.
Rachel
Instead of being able to see the wisdom in that, that having access to food while sitting in a hospital room is so wise and comforting. If we were neutral about food and body size, then it would be like, okay, bring all the croissants, and have as many as you want, and comfort yourself and try to get through this really horrific time. Instead, we hold up some coping mechanisms and vilify others, which is ridiculous.
Virginia
I will say, for the people in my life listening to this, that I did have people who supported me on the croissants and understood when I said, “No, I really can’t. Yes, my husband can leave and go for a run, and that’s really helping him through this time, but me leaving is not something that will feel—like, that feels terrifying.” And people did respect that, but it was tricky to articulate. And it’s tricky that when you’re in the active experience of trauma, to have to articulate your need and defend a need. You shouldn’t have to assert to other people that your need is valuable at that point.
Rachel
Right, you shouldn’t have to defend it. Even just thinking over the past year and a half with COVID, there is some subset of people who have coped by eating, and there is some subset of people who have coped by restricting. And we don’t name the restriction as harmful. We praise it when really, restriction weakens your immune system and makes you more vulnerable to stress and the impact of stress. But instead, what we say is, oh, if somebody is restricting and losing weight, that that’s a positive thing. We don’t name the harm of it, where, you know, eating to cope actually makes a lot of sense. And is way more beneficial than restricting.
Virginia
Because that’s at least meeting a physical need. It’s getting you through. Absolutely.
So, we see the weight stigma showing up in the active trauma space, and as people are kind of navigating coping strategies. And then we also see it, you know, I don’t want to say after, because of course, trauma can be a long unfolding process, but in terms of how these fat bodies are then pathologized by the world, right? So talk a little bit about what is often the approach to when, you know, whether it’s in eating disorder treatment, or in trauma therapy, in general, when you know, providers encounter someone in a bigger body, and the focus goes to weight loss, and why that is not actually going to help with the healing from the trauma.
Rachel
What I often hear and see from clients is, there’s two paths that come up the most: I see clients who went to therapy, are in a fat body, and the provider made an assumption that because they’re fat, they must have had trauma, without even assessing or asking questions. And then there’s clients who do connect their fatness to trauma, and so they have gone to therapy, wanting to talk about their trauma history, and sometimes also starting out in therapy saying, and I would like to lose weight, or just not even focusing at all on body size, but just wanting to talk about their trauma. And what happens is that therapists then say, “Well, yes, we can work on your trauma. And if we work on your trauma, then you’ll lose weight.” Because if we’ve decided that eating in response to trauma lead to weight gain, then the belief is, if we heal your trauma, then your eating is gonna change, and you’ll release the weight. That’s the word that comes up.
Virginia
That phrase is really yucky.
Rachel
It seems to be the one that my clients hear quite frequently. People are in fat bodies for endless reasons. There are so many different reasons, and we don’t need to know them in order to know that promoting weight loss is harmful. It doesn’t matter if somebody is fat because of trauma, or for any of the other reasons that influence body size. It’s not like diets differentiate, that one diet says, okay, this person had trauma, so, this diet is effective.
Virginia
I can totally see the trauma diet becoming some new creepy trend on Instagram: Intermittent fasting to heal your inner child or something.
It’s just so missing the point because it’s not helping people work on, you know, processing what’s really happened to them or figuring out what they really need. It’s like solving this problem that’s, as you say, possibly related, possibly even completely unrelated, and not actually a problem at all. And giving them this other thing to focus on and then measure their “success” based on whether they can control it or not.
Rachel
I think it’s so important to name really clearly that fatness is not the trauma. Weight stigma is a trauma, and clients have all kinds of other traumas that they’re coming in with. But fatness is not the trauma, and trying to you know “fix fatness” is actually re-traumatizing. So if somebody is coming in, and a therapist is saying, '“Okay, I’m going to help you with your trauma, and I’m going to help you lose weight,” they’re actually re-traumatizing somebody who’s already been through significant trauma.
Virginia
So where do you think that sort of line of thinking in the provider community is coming from? I mean, why? Why is that an accepted practice when it’s so clearly causing harm?
Rachel
It’s an important question. I think some of it is that providers are still being trained in really stigmatizing programs. I don’t think people are learning about the impact of anti-fat bias and weight stigma. I think, unfortunately, a lot of providers haven’t done their own work around it, so they may still be trying to suppress their own weight or still trying to diet in their own life. As providers, we’re always going to be in process. It’s not that, you know, as a therapist, you suddenly get to this place where you’ve worked through everything.
But I think if we haven’t done our own work around weight stigma and our relationship with our body, then we are likely to harm clients that are coming in wanting to address those issues. I think the trauma field still supports this, I think some of it comes from the eating disorder field. But I think a lot of it comes from the trauma field. If you read some of the main books about trauma, this narrative is written about, and they are not HAES-informed books. So if you don’t already have some footing in Health at Every Size, and you’re looking for a trauma book to read, or to learn about, that narrative is going to be reinforced.
Virginia
It also makes me think about how much our internalized vision of healthy or recovered or happy is intrinsically linked to thinness, so if someone achieves weight loss—however temporary that’s likely to be, and no matter what they have to do in order to achieve it—we’re going to view that as “success,” because that narrative is so embedded in our culture. And we’re not going to look deeper than that, we’re not going to see that that isn’t actually dealing with the underlying issues.
Do you think there’s a degree to which the underlying stuff feels harder, you know, that it’s that work that might be scarier to people? And going on a diet feels like, well, this is what I can control. So let me do that.
Rachel
Absolutely. I mean, I think that all of us have been socialized to believe that weight is under our control. And that if we can just find the right diet and lose weight, then it’s going to solve other problems. And there’s so many providers who reinforce that.
Virginia
And the science that’s getting done is reinforcing this, too. I mean, I was looking at a couple of studies that were done recently on adverse childhood experiences, and they are all trying to document this phenomenon. One is called “Adverse childhood experiences are associated with an increased risk of obesity and early adolescence.” (I apologize for using the O-word, I’m quoting the fatphobic research.) And there are several others I’ll link to in the transcript. It seems like the goal of this research is to say, we should worry about childhood trauma because people might get fat from it, as if that is the outcome we’re worried about, not the trauma.
I’m curious for your thoughts on that research, I think we see the similar thing happening in research on childhood poverty and childhood hunger. Like if fat is the outcome, then it’s really bad.
Rachel
I think that we want to believe that research is objective and neutral. And the truth is that it’s not. The questions that are being asked in these research studies are inherently biased. And so they are asking a question that they think they know the answer to. I would love to sit down with somebody like Deb Burgard or somebody who’s really great at pulling through statistics, because just glancing at this research, I’m not sure that there’s actually a difference between the percentage of kids who are in higher weight bodies in this study where they’re connecting it to adverse childhood experiences, and just the percentage of kids who are in higher weight bodies in general.
Virginia
Oh, that's interesting. Yeah.
Rachel
So I’d be really curious for somebody who’s really great at statistics to kind of pull all of that apart.
Virginia
Yeah, because if it’s like we’re trying, what it feels like, in a way is that they’re looking at the “childhood obesity epidemic.” They’re saying kids are in bigger bodies now, let’s find this explanation for it. And then that’s a way of pathologizing the fact that kids come in different sizes. Then you’ve decided, all those kids are traumatized or broken in some way. Now, you’ve explained it to yourself. Just yeah, that’s a pretty fatphobic way of going about the problem.
Rachel
Right. And it’s like you said, I mean: You’re identifying fatness as the problem, like, how about if we identify the problem is that so many kids have childhood trauma? This idea that, a kid’s coming in and identifying that they’ve had a history of physical abuse, sexual abuse, and the thing that these studies are worried about is fatness?!
It’s just so harmful. And it’s scary that this is how we’re responding to kids’ body size and to trauma, that the thing that these studies are focused on and asking questions about is how do we make kids not be in bigger bodies? And ignoring like, how do we protect kids from being physically and sexually abused?
Virginia
Right, right. It’s a really similar thing that played out in childhood hunger research, which was like, in order to get funding and attention on childhood hunger and childhood poverty, there was a huge effort to document the connections to higher weight. And it’s like, do I really need to explain to you, that you should care about kids being hungry? You needed some other outcome—you needed to make it about fatness? In order to care about this problem? We couldn’t just care about feeding hungry kids? It’s mind blowing. And it feels very similar.
This also feels very tied to the older conversation about whether “obesity” should be classified as a disease. And, a lot of folks who were in favor of that argued that it would reduce stigma, if we could understand high body weight as a “chronic condition” because you would understand that it was beyond people’s control, and they needed intervention and support. That has definitely not been the result of classifying obesity as a disease. We know that it has only furthered weight stigma, and it feels like a similar parallel here that if we’re trying to understand weight as always trauma related. You could argue that that’s a way of increasing empathy. But it doesn’t seem like that’s how that conversation plays out.
Rachel
Yeah, I am fascinated by this kind of line of thinking. I really am curious about who thought it was a good idea to classify body size as a disease. And like, how they convinced themselves that that was actually going to decrease stigma or not pathologize people. I understand the narrative they’re telling themselves but I would love to dig deeper and really pick apart like, what actually is going through their mind when they thought that that was a good idea.
Of course labeling body size as a disease was not going decrease stigma. I think, first of all, it contributes to the idea, like when we think disease states, we think of something that requires treatment. And so then you’re reinforcing that body size needs some sort of intervention. So naming it as a disease is not going to reduce the stigma in the culture, like we actually have to address the stigma and not try to find creative ways to describe body size, and pretend that that’s actually going to be the thing that’s beneficial. We have to find ways to reduce stigma. I’m just sick in general of our need to pathologize these expected and typical responses to being in a body, and being in a culture that harms bodies.
I think this happens with lots of different diagnoses. I don’t think this is unique to labeling body sizes as disease, but I think we’ve just got to get away from pathologizing people and name the problem in the culture and you know, in the environment, instead of saying that body size is the problem.
Virginia
Completely agree. And on the other side of this conversation, what we sort of started touching on in the beginning that I just want to hit on quickly, before we wrap up, is that it makes it harder for people to talk about what’s happened to them, because they’re worried if they own their full story, that they’re going to be pathologized for their weight. And I do sometimes feel within the Health at Every Size community, we don’t do a great job of making space for this story, right? Because we’re so quick to fight against the pathologizing. Then I hear from folks in fat bodies that feel like, I’m not allowed to be a fat person with health problems here. So I don’t know if you have any thoughts about that, because I’m sure you sort of see that tension, often.
Rachel
Totally. And it makes sense to me, I understand why that’s the reaction from the Health at Every Size community. When you’ve been oppressed for so long, and there’s such a difficult time holding nuance within the larger environment, that anytime there’s a narrative, that there’s a fear it’s going to increase oppression or marginalization, of course, people want to defend and protect against it. So it makes a lot of sense to me. But what it does create is this reinforcing of stigma and it silences people. And we want to do the opposite within the Health at Every Size community, we want everybody’s story to be able to be told. So I think we have to be able to hold space for these conversations. Because, one, they’re true, right? Like this is real. These narratives are true and real. There’s a ton of nuance within the research around, you know, fatness and health conditions that we need to be able to talk about. And when we don’t talk about them, we prevent people from getting help with the things that there actually are interventions for, and weight loss is not one of them. If somebody in a fat body can’t talk about whatever health conditions they might be dealing with, then how are they going to get appropriate interventions for whatever those health conditions are? So we’ve got to be able to talk about it.
Virginia
That makes total sense. And I am so grateful for how you articulate this nuance. Thank you so much for your work and for being here.
Rachel
Thanks for having me on for these hard conversations.
Virginia
They are hard but they’re really important and I hope it helps people feel more seen in their own experiences and more like they can own their stories.
Thank you all so much for listening to Burnt Toast! If you like this episode and you aren’t yet subscribed, please do so.
If you are a subscriber, thank you so much for being here. And please consider sharing Burnt Toast on social media or forwarding it to a friend.
Burnt Toast transcripts and essays are edited and formatted by Jessica McKenzie, who writes the fantastic Substack, Pinch of Dirt. Our logo is by Deanna Lowe.
And I’m Virginia Sole-Smith. You can find more of my work at virginiasolesmith.com or come say hi on Instagram and Twitter. I’m @v_solesmith. I’m barely on Facebook anymore, so don’t worry about that. Thanks for listening and talk to you soon!















Share this post